How Long Fentanyl Stays In Your System
How Long Fentanyl Stays In Your System How Long Fentanyl Stays in Your System Introduction Understanding how long fentanyl stays in your system is important for anyone affected by fentanyl use, substance abuse, or the opioid epidemic. Many people ask this question because fentanyl is a powerful opioid with high potency, fast absorption, and a long detection window in the body. At Sullivan Recovery in Mission Viejo, we help each patient learn how fentanyl impacts the brain, body, and mental health while offering effective outpatient fentanyl addiction treatment that supports long-term recovery. What Fentanyl Is and Why It Stays in the Body Fentanyl is a synthetic analgesic used to treat severe pain. It is stronger than morphine, which is why doctors prescribe it in controlled dose forms such as tablet, nasal spray, injection, and transdermal patch applications. Because of its strength, fentanyl binds to the opioid receptor quickly, and this binding slows natural metabolism, allowing the drug to stay in the body longer than many other opioids. The body stores fentanyl in fat tissue due to its chemical structure. This increases the total amount of time it can remain active and detectable during a drug test. Factors like liver function, body weight, and use frequency all influence how long fentanyl stays in your system. These factors also play a role in the symptoms someone may experience during fentanyl addiction treatment at Sullivan Recovery. How the Body Processes Fentanyl The liver breaks down fentanyl before the body removes it through urine, sweat, or saliva. Slow liver function can extend the detection window and increase the chance of side effect problems such as nausea, diarrhea, insomnia, and anxiety. Many individuals experience shifts in blood pressure or other health changes because fentanyl affects the central nervous system and the brain’s opioid signaling. Because fentanyl impacts both body and mental health, many people need therapy or coping support to manage symptoms linked to substance abuse or addiction. Sullivan Recovery offers outpatient programs that help patients stabilize health while they address emotional stress, cravings, and relapse risks associated with fentanyl. How Long Fentanyl Stays in Your System The length of time fentanyl remains detectable varies by testing method. Each type of test has a different sensitivity based on the kind of sample collected. Urine Testing A urine drug test is the most common method. It can detect fentanyl for 1 to 3 days after the last use. Heavy or frequent use may extend the detection window because fentanyl accumulates in fat cells. Urine testing is common in outpatient rehab settings, including fentanyl addiction treatment at Sullivan Recovery. Blood Testing A blood test shows fentanyl for a shorter period, usually up to 12 hours. Blood testing is mainly used in emergency situations when a patient shows signs of overdose or other health complications. Hospitals may also use naloxone in these cases because it blocks the opioid receptor and helps reverse overdose effects. Saliva Testing Saliva and saliva testing can detect fentanyl for 1 to 2 days, but accuracy varies. Moisture levels in the nose and mouth, medication use, and individual metabolism may change results. This method is less common but may appear in some workplace testing programs. Hair Testing Hair tests can detect fentanyl for up to 90 days. This is the longest detection window available for any drug test. However, it does not help with short-term monitoring because it takes weeks for fentanyl to appear in the hair strand. Why Fentanyl Stays in the System Longer Than Other Opioids Fentanyl attaches tightly to the opioid receptor, which slows down how fast the body can remove it. Its high potency increases the strain on the liver and reduces metabolism efficiency, especially for individuals with pre-existing health issues. The fat-soluble nature of fentanyl also plays a major role because the drug sits in fat tissue and is released over time. These factors explain why people entering fentanyl addiction treatment may still test positive for several days. Sullivan Recovery provides structured outpatient therapy that helps each patient learn coping tools for cravings and withdrawal while monitoring physical health. Forms of Fentanyl and Their Detection Times Different fentanyl products affect the body in different ways: Injection An injection reaches the bloodstream fast and increases overdose risk. It may be detectable for 12 hours in blood and up to several days in urine. Nasal Spray A nasal spray absorbs through the nose lining. Some patients feel its effects quickly, and the body may detect it for 1 to 2 days. Transdermal Patch A transdermal patch releases medication through the skin slowly. This keeps fentanyl in the bloodstream longer, increasing the detection window. Tablet A tablet dissolves in the mouth or stomach. It may stay detectable for multiple days depending on dose and frequency. These differences matter when a patient enters fentanyl addiction treatment at Sullivan Recovery because the treatment team evaluates each form of exposure when building a recovery plan. Side Effects While Fentanyl Is in the Body Fentanyl affects both mental and physical health. Many individuals experience nausea, diarrhea, changes in blood pressure, and shifts in sleep. Others develop insomnia, anxiety, and confusion due to how fentanyl interacts with the brain. These reactions may occur even after a short dose or when using fentanyl as a medication. People with substance abuse concerns may feel stronger effects because fentanyl creates changes in brain chemistry. Over time, the body becomes dependent on fentanyl, increasing the risk of addiction, overdose, and health decline. Sullivan Recovery helps patients address these symptoms through outpatient therapy, mental health support, and optional medication management for cravings. Fentanyl Withdrawal and Detection Overlap A person may begin to experience withdrawal even while fentanyl still appears in a drug test. Withdrawal may cause sweating, anxiety, insomnia, nausea, diarrhea, or increased pain sensitivity. These symptoms show that the body is removing fentanyl and resetting opioid receptor function. Some patients benefit from medications like methadone, used to stabilize the opioid receptor and reduce withdrawal stress. Methadone does not remove fentanyl
Fentanyl What Is It Used For

Fentanyl What Is It Used For Fentanyl What Is It Used For: Full Guide to Medical and Non-Medical Risks Understanding fentanyl what is it used for is important for anyone who wants clear information about this powerful opioid. Fentanyl is a synthetic opioid medication that treats severe pain when other options fail. It can help patients in hospitals, but misuse can create serious health risks, overdose, and the need for quick medical action with naloxone. Knowing how fentanyl works helps people understand safe dose limits, legal use, and why so many emergency department visits are linked to this drug. At Sullivan Recovery, we help individuals who struggle with fentanyl misuse through structured outpatient treatment and safe recovery support. What Fentanyl Is and How It Works Fentanyl is a strong opioid medication that changes how the brain responds to pain. Doctors prescribe it when a patient experiences severe pain that does not improve with standard medication. Hospitals use fentanyl in controlled doses during surgery, after surgery, or for advanced medical conditions. Synthetic production makes fentanyl fast-acting and highly potent. It binds to opioid receptors quickly, which creates relief within minutes. Because of this increased strength, the risk of overdose grows when the dose is not carefully monitored. Fentanyl What Is It Used For in Medical Settings Doctors use fentanyl during surgical procedures to manage pain and help stabilize a patient’s condition. The medication can be given through injection, which allows the dose to be controlled with precision. Hospitals also use fentanyl in the emergency department when a patient arrives with severe trauma. Cancer patients may receive fentanyl to ease advanced pain symptoms. Some individuals use a fentanyl tablet or nasal spray under medical supervision. These forms act fast and help reduce breakthrough pain. Different Forms of Fentanyl Fentanyl comes in several forms depending on the patient’s needs. An injection is common in hospitals because it works fast and allows for controlled dosing. A tablet or nasal spray is used when a patient needs relief outside surgical care. Fentanyl patches release medication slowly throughout the day. This method supports long-term pain control for patients with chronic medical issues. Each form has strict guidelines to prevent increased risk of overdose. Why Fentanyl Misuse Has Increased Non-medical fentanyl misuse has increased over the past decade. Illicit fentanyl is often mixed into street drugs to increase potency, which leads to unpredictable dose levels. Many individuals do not know fentanyl is present, which raises overdose risks. Overdose cases involving fentanyl now appear in nearly every emergency department nationwide. These visits often require quick naloxone use to reverse the effects. Even a small amount of fentanyl can shut down breathing within minutes. How a Dose of Fentanyl Affects the Body A dose of fentanyl can relax the body and reduce pain fast. The drug lowers brain activity in areas related to pain signals. However, high doses slow breathing, which can cause life-threatening symptoms. Fentanyl can cause dizziness, drowsiness, or confusion when the dose is too strong. Many overdose cases occur because street drugs include increased fentanyl levels. This creates unpredictable reactions that require emergency care. The Role of Naloxone in Fentanyl Overdose Naloxone is a medication that reverses the effects of fentanyl. It attaches to opioid receptors and blocks fentanyl from shutting down the body’s breathing. Emergency department staff use naloxone often because fentanyl overdoses have increased sharply. Naloxone can be given as an injection or nasal spray. The nasal spray allows quick use outside a hospital, even by bystanders or family members. Multiple doses may be required when fentanyl levels are high. Signs of Fentanyl Misuse Fentanyl misuse may cause sudden changes in behavior, mood, or physical health. People may appear extremely drowsy, confused, or unable to stay awake. Slow breathing is one of the most serious warning signs. Other signs include pinpoint pupils, nausea, and weak coordination. Fentanyl misuse often leads to repeated emergency department visits. When these patterns appear, a structured treatment program is needed. Risks Linked to Illicit Fentanyl Use Illicit fentanyl is dangerous because it contains no controlled dose. Street products may contain increased concentrations that the individual cannot detect. This leads to overdose situations where naloxone is needed right away. Many illicit drug markets sell fentanyl in powder, tablet, or nasal spray forms. These forms are unpredictable and often mixed with other substances. Users face a high risk of respiratory failure in minutes. Why Fentanyl Addiction Happens Quickly Fentanyl addiction develops fast because the opioid creates strong effects in the brain. The drug increases dopamine levels, which creates a short sense of relief and comfort. The brain begins to crave the medication when the dose wears off. Repeated misuse changes how the body responds to pain and stress. Over time, a person may use fentanyl only to avoid withdrawal symptoms. This pattern requires medical support and structured outpatient rehab. Medical Fentanyl vs. Illicit Fentanyl Medical fentanyl is produced in regulated environments with strict dose control. Hospitals use the drug with trained staff who monitor breathing and heart rate. This creates a safer setting for pain treatment. Illicit fentanyl is made without safety standards. Users cannot track the dose, purity, or ingredients. This leads to increased overdose rates that often require emergency department treatment. What Happens During a Fentanyl Overdose During a fentanyl overdose, breathing slows or stops. The person may lose consciousness and show no response to loud sounds or touch. Skin may turn pale or blue as oxygen levels drop. Naloxone must be given quickly to reverse the opioid effects. After naloxone, emergency staff often provide oxygen support and monitor vital signs. Overdose survivors may need long-term addiction treatment. How Sullivan Recovery Helps With Fentanyl Misuse Sullivan Recovery provides outpatient treatment for individuals struggling with fentanyl misuse. Our program helps people manage withdrawal symptoms and reduce cravings in a safe setting. Many clients choose outpatient rehab because it allows them to continue work, family life, and personal responsibilities. We focus on therapy, medication support, and structured recovery planning. Our
When To Go To Rehab For Alcohol

When To Go To Rehab For Alcohol When To Go To Rehab For Alcohol: A Clear Guide for Knowing the Right Time Understanding when to go to rehab for alcohol can feel confusing for many people. Alcohol misuse often builds slowly, and people may hide signs of substance abuse even from themselves. This blog explains when to go to rehab for alcohol, what symptoms signal the need for help, and how Sullivan Recovery in Mission Viejo supports people seeking safe and effective outpatient treatment. As people face addiction, anxiety, relapse patterns, and changes in behavior, professional care from a trusted treatment center becomes a key step toward long-term health. At Sullivan Recovery, we help individuals address alcohol misuse through therapy, medication support, mental health treatment, and structured outpatient rehab. Our clinical team uses proven recovery methods to help people rebuild their lives with effective coping tools and strong relapse-prevention plans. Once someone knows when to go to rehab for alcohol, they can enter treatment early and reduce the risks linked to drinking, substances, and harmful behavior. Signs Alcohol Use Is Becoming a Problem Many people do not realize their alcohol intake has changed until it affects daily functioning. Increased drinking, loss of control, and withdrawal symptoms are common signs of worsening substance abuse. These patterns may lead to poor physical health, unstable behavior, and emotional strain. People often experience anxiety, trouble coping, or changes in mood when alcohol becomes a primary focus. Alcohol may replace important activities, relationships, or responsibilities. Once a person relies on alcohol to function or feel “normal,” treatment becomes necessary. How Alcohol Impacts Mental Health and Behavior Alcohol use can create significant shifts in mental health. Many people notice increased anxiety, depression, or sudden mood swings due to changes in brain chemistry. These symptoms make it harder to manage daily stress or maintain healthy behavior. Alcohol also affects impulse control and emotional balance. This can lead to conflict at home, problems at work, or risky decisions involving substances or drug use. If emotional stability begins to depend on drinking, that is a strong indicator of when to go to rehab for alcohol. Physical Health Symptoms That Signal the Need for Rehab Alcohol affects the brain, liver, and overall health. Frequent drinking can cause sleep problems, high blood pressure, and weakened immune response. Many people also experience trembling, sweating, or nausea when they try to stop drinking. These physical symptoms show the body is dependent on alcohol. When physical withdrawal begins, entering a treatment center helps reduce medical risks. Sullivan Recovery offers medical oversight, nursing support, and health monitoring to guide people safely through the early stages of quitting alcohol. Dual Diagnosis and Co-Occurring Disorders Some people experience both addiction and mental health conditions at the same time. This is known as dual diagnosis. Common examples include anxiety disorders, depressive symptoms, and stress-related conditions that worsen with drinking. A person with dual diagnosis needs more than simple detox. They need therapy, medication support, and a treatment provider who understands how both conditions interact. Sullivan Recovery provides structured outpatient rehab services to treat alcohol misuse and mental health needs at the same time. When emotional symptoms worsen with alcohol use, that is a clear signal for when to go to rehab for alcohol. When Drinking Affects Daily Functioning If someone’s drink habits begin to interfere with responsibilities, treatment is often necessary. People may miss work, cancel plans, or stop engaging with family. Bills may go unpaid, and important tasks may be ignored. These changes often occur because alcohol takes priority over everyday life. Once drinking becomes the focus, therapy and structured treatment can help restore stability and well-being. Outpatient rehab offers support while allowing people to remain active in their daily routine. The Role of Therapy in Alcohol Treatment Therapy helps people understand why they drink and how alcohol affects their behavior. A therapist teaches coping techniques that reduce stress, regulate emotions, and prevent relapse. Many people also learn how anxiety and past experiences influence their drinking patterns. At Sullivan Recovery, we use proven therapy methods to support healing and long-term sobriety. Our sessions address both substance abuse and mental health concerns. When someone struggles to stop drinking on their own, therapy becomes an important part of knowing when to go to rehab for alcohol. How Medication Helps Support Recovery Some people benefit from medication during alcohol recovery. Medication can reduce cravings, ease withdrawal symptoms, and support emotional balance. These tools help stabilize the brain as it adjusts to life without alcohol. A physician or nurse practitioner may prescribe medications based on individual needs. Medication works best when combined with therapy and structured treatment programs. Sullivan Recovery offers medication support within its outpatient rehab, giving patients full evidence-based care. What Happens in Outpatient Rehab Outpatient rehab is flexible and supportive. People attend scheduled therapy sessions, group meetings, and educational classes while still living at home. This gives patients a chance to practice coping skills in real life while receiving ongoing guidance. Sullivan Recovery provides outpatient rehab that focuses on therapy, mental health treatment, relapse prevention, and medication support. Nursing and clinical staff help patients learn new skills, maintain stability, and manage the stresses that contributed to drinking. Many people choose outpatient rehab because it allows them to get help without leaving work or family. Comparing Inpatient and Outpatient Treatment Inpatient rehab provides 24-hour supervision for people with severe alcohol addiction. Patients stay at the treatment center full-time and participate in structured programs. This level of care is ideal for those at risk of dangerous withdrawal or repeated relapse. Outpatient rehab allows people to receive treatment while managing daily responsibilities. Sullivan Recovery specializes in outpatient care, offering therapy and mental health support without requiring overnight stays. This model works well for those seeking ongoing care after detox or those with moderate symptoms. How Relapse Happens and Why Support Helps Relapse often occurs when a person struggles with stress, lack of coping tools, or emotional triggers. Alcohol cravings can
What Do They Do In Alcohol Rehab
What Do They Do In Alcohol Rehab What Do They Do in Alcohol Rehab? Introduction People often ask, “what do they do in alcohol rehab?” because they want clear information before seeking help. Understanding this process can reduce fear and give a patient more confidence before entering a treatment center. Alcohol rehab centers use structured treatment programs to help individuals stop drinking, manage substance abuse issues, and rebuild health. When people search for what do they do in alcohol rehab, they want to know what happens day-to-day inside treatment centers and how treatment programs guide someone toward sobriety. Rehab centers focus on addiction treatment, therapy, detox, and long-term relapse prevention. This blog explains the full rehabilitation process, including the role of medication, therapy, education, and mental health support. What Do They Do in Alcohol Rehab? Alcohol rehab centers help patients regain control of their health by treating addiction as a disease that affects the brain, behavior, and emotions. When learning what do they do in alcohol rehab, it helps to know that patients receive detox, therapy, education, and daily support. Each treatment provider focuses on improving coping skills, stabilizing mental health, and guiding the patient through each step of the recovery model. Most treatment centers use licensed physicians, nurses, and mental health professionals to monitor symptoms and create a stable path toward sobriety. Rehab programs often include inpatient, outpatient, and PHP levels of care, depending on the drinking problem and the intensity of symptoms. Every patient receives structured information that teaches them how to manage cravings, regulate emotion, and rebuild their physical and mental health. Detox and Medical Stabilization The rehabilitation process usually starts with detox. Detox helps remove alcohol from the body under supervision from a physician or trained health professional. This stage is important because withdrawal can affect the brain, mind, emotion, anxiety levels, and overall health. During detox, patients may receive medication like naltrexone to reduce cravings and stabilize behavior. A treatment provider monitors hydration, hygiene, sleep, and vital signs to reduce health risks. Removing alcohol safely prepares the patient for the next stages of therapy and treatment programs. Assessment and Treatment Planning After detox, the treatment center performs a full assessment. This assessment looks at mental health, substance abuse history, drinking patterns, and any signs of dual diagnosis. A dual diagnosis occurs when a patient has both addiction and another mental health disorder such as anxiety or depression. The information gathered helps the treatment provider build an individualized program. This program may involve medication, therapy, education, and structured support from rehab centers. By customizing treatment, the center can help the patient strengthen coping skills and prevent relapse. Therapy in Alcohol Rehab Therapy is a major part of what they do in alcohol rehab. Individual therapy helps patients understand their drinking problem and the behavior connected to addiction. Group therapy creates community support, which helps reduce isolation and improve long-term engagement in treatment. Patients learn coping methods to manage stress, emotion, and cravings. Therapy sessions may explore how substance abuse affects the mind, brain, relationships, and daily functioning. Common therapy methods include cognitive therapy, art therapy, meditation practices, and behavioral approaches that help patients build new habits. Mental Health and Dual Diagnosis Treatment Mental health treatment is essential in many treatment centers. Patients with dual diagnosis require medication, therapy, and education to stabilize symptoms linked to anxiety, depression, or other disorders. This approach improves behavior regulation and supports long-term sobriety. Mental health professionals teach coping techniques that help regulate the mind and emotions. Treatment providers also monitor medication and track how different symptoms respond to therapy. This support helps each patient stay balanced and committed to healthier drinking behavior. The Role of Medication in Rehab Medication can be part of treatment programs for addiction. Physicians often use naltrexone or other approved medication to reduce cravings or stabilize mental health symptoms. Medication supports the patient during the rehabilitation process, especially when withdrawal or cravings create pressure to drink. In alcohol rehab centers, medication is used in combination with therapy, education, and outpatient rehab services. It is monitored daily by a health professional to ensure safety. Patients receive information about how medication works and how it supports sobriety. Education and Skill Building Education is an important part of what they do in alcohol rehab. Patients receive information about how drinking affects the brain, health, and behavior. Understanding addiction as a disease helps each patient stay committed to treatment. Skill-building sessions teach coping tools for stress, anxiety, and emotion management. Education classes also cover relapse prevention, daily hygiene routines, and the importance of community support. These programs help patients regain confidence and prepare for life after treatment. Inpatient Treatment Structure Inpatient treatment centers provide 24-hour care inside the facility. Patients follow a structured daily schedule that includes therapy, group sessions, medical monitoring, and personal development programs. The controlled environment helps maintain sobriety during early recovery. Patients in inpatient rehab receive multiple types of therapy, participate in meditation exercises, and engage in art therapy or activity-based programs. Inpatient treatment is recommended for individuals with a severe drinking problem or when health risks require close monitoring. This level of care supports stability before transitioning into outpatient programs. Outpatient and PHP Programs Outpatient rehab offers flexibility for patients who do not require inpatient care. Outpatient programs allow patients to receive treatment while living at home, which can help them practice coping skills in real-life situations. Outpatient treatment still includes therapy, medication support, education, and regular check-ins with a treatment provider. PHP (Partial Hospitalization Program) is a structured level of outpatient care for those who need more support than standard outpatient sessions. PHP programs provide full-day treatment at the center but allow patients to return home each evening. Both outpatient and PHP options support ongoing sobriety and reduce relapse risk. Therapeutic Activities and Healing Practices Many rehab centers use art therapy, meditation, and mindfulness exercises to help the mind and emotions heal. These practices support mental clarity and reduce anxiety. Creative programs help
Does Insurance Cover Alcohol Rehab

Does insurance cover alcohol rehab? Learn what major plans like Aetna and Blue Cross cover, costs, and how Sullivan Recovery makes treatment affordable.
Does Medicare Cover Alcohol Rehab
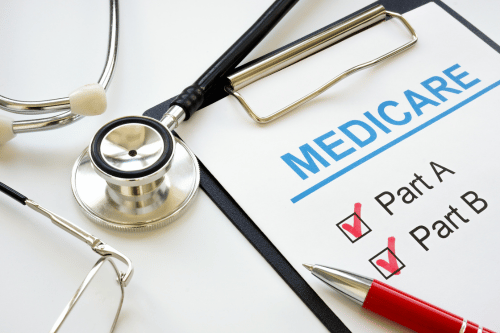
Learn how Medicare covers alcohol rehab, inpatient & outpatient treatment, medications, and mental health services to support addiction recovery.
How Effective Is Rehab For Alcoholism

Discover how effective rehab for alcoholism is. Learn about treatment success rates, therapy, medication, and recovery options at Missouri Behavioral Health.
How Much Is Alcohol Rehab
Discover how much is alcohol rehab, what affects the cost, and ways to afford treatment. Learn about insurance, payment plans, and affordable recovery options.
What Does Alcohol Rehab Cost
Discover what does alcohol rehab cost, key price factors, and insurance options. Learn how Sullivan Recovery makes treatment affordable in Mission Viejo.
How Long Is Alcohol Rehab

Wondering how long is alcohol rehab? Learn what affects recovery time, program options, and how Sullivan Recovery helps patients achieve lasting sobriety.
