TMS Therapy Side Effects: What You Need to Know
Table of Contents Seeking Drug Or Alcohol Detox? Sullivan Recovery is a leading drug and alcohol detox in Mission Viejo, California. Call Today! Clinically Reviewed By: Rachel Sweet | LMFT TMS Therapy Side Effects: What You Need to Know What Is TMS Therapy? Transcranial Magnetic Stimulation (TMS) is a noninvasive treatment for patients with treatment-resistant depression and other mental health conditions such as obsessive-compulsive disorder (OCD) and post-traumatic stress disorder (PTSD). This non-invasive treatment method uses an electromagnetic coil to deliver magnetic pulses to targeted brain regions, particularly the prefrontal cortex, which is responsible for mood regulation and brain activity. TMS therapy is considered a safe option for those who have not responded to antidepressant medications or other forms of treatment. Unlike electroconvulsive therapy (ECT), which can cause severe cognitive side effects, TMS does not require anesthesia and has minimal side effects. Common Side Effects of TMS Therapy While TMS is an effective treatment for major depression and other psychiatric disorders, some potential side effects can occur. Mild Side Effects Patients commonly experience mild discomfort, scalp pain, or facial twitching during the initial sessions. These therapy side effects are usually temporary and improve as weeks of treatment progress. Some may also experience jaw pain, neck pain, or facial pain due to the muscle contractions caused by the magnetic stimulation of nerve cells. Moderate Side Effects Some individuals report cognitive side effects, such as temporary cognitive function changes, including mild memory issues or difficulty concentrating. Other moderate effects include auditory processing sensitivity due to the noise during treatment, as well as hearing issues, particularly for patients without proper ear protection. Serious Side Effects Though rare, TMS therapy carries a risk of seizures, particularly in individuals with a history of epilepsy or a seizure disorder. Other adverse events may include hypomanic symptoms in patients with bipolar disorder or an increase in OCD symptoms for those undergoing rTMS treatment for compulsive disorders. Individuals with a family history of seizures or preexisting conditions such as brain tumors or aneurysm coils should consult a healthcare provider before beginning treatment. Mechanism of Action TMS therapy works by stimulating brain cells using electromagnetic pulses, which target the brain responsible for mood control. The electrical stimulation provided by the treatment coil influences neural pathways in the motor cortex and prefrontal cortex, leading to changes in brain function that help alleviate depressive symptoms. Types of TMS Therapy Repetitive TMS (rTMS) This treatment method involves a pulse train of magnetic waves delivered to the prefrontal cortex. rTMS treatment is commonly used for treatment of depression and has shown an impressive success rate in patients with severe depression. Deep TMS (dTMS) Deep TMS uses a specially designed treatment coil to reach deep brain stimulators, targeting areas associated with OCD symptoms and depressive disorder. This method allows for deeper magnetic stimulation, which can be beneficial for individuals with treatment-resistant depression. Understanding Eligibility for TMS Therapy Criteria for Patients Patients with depression who have not responded to at least two antidepressant treatments may be eligible for TMS. However, patients with implants controlled by electronic devices, such as cochlear implants, cardioverter defibrillators, vagus nerve stimulators, or deep brain stimulators, should avoid TMS due to potential risks from the electromagnetic pulses interfering with these medical devices. Considerations for Specific Conditions Individuals with metal devices in the head, such as metal plates, dental fillings, aneurysm clips, aneurysm coils, or bullet fragments, may face additional risks. Pregnant women and elderly patients should also consult a healthcare provider before considering TMS therapy. Treatment Schedule and Expectations A treatment plan typically consists of weeks of treatment, with a week of treatment involving five therapy sessions. Each treatment session lasts 20 to 40 minutes, depending on the pulse strength and individual response. The clinical response varies, with some experiencing relief in depression symptoms within the first few weeks, while others require additional treatments. Safety Precautions Before Starting TMS Patients should undergo a medical history review before starting TMS therapy. Those with a history of seizures, brain stents, or motor dysfunction need to be assessed for potential long-term effects. Proper ear protection is essential to prevent hearing loss due to the ambient noises created by the electromagnetic coil. Managing Side Effects During TMS For scalp discomfort and scalp pain, adjusting the treatment coil placement can reduce patient discomfort. Counter pain relievers such as over-the-counter pain medication can help with headaches and muscle contractions. Individuals experiencing cognitive function issues should discuss any adverse effects with their consulting provider. Comparing TMS Therapy to Other Treatments Medications TMS therapy provides an effective depression treatment without the adverse side effects of depression medications. Many patients with treatment-resistant depression opt for TMS after experiencing antidepressant side effects such as weight gain, negative side effects, or effects of medications on daily activities. Psychotherapy While psychotherapy is an important part of mental health treatment, it may not be sufficient for patients with severe depression. Combining TMS therapy with therapy sessions can enhance emotional responses and improve the success rate of depression treatments. Alternative Therapies Other treatment options include electrical activity-based treatments, magnetic resonance imaging-guided therapies, and holistic approaches like lifestyle changes. However, TMS therapy remains one of the most effective treatments for mental illness and depressive disorder. Conclusion and Considerations for Patients TMS therapy is an effective treatment for patients with depression who have not responded to standard antidepressant treatments. With a personalized approach, this noninvasive procedure offers life-changing results for those struggling with mental health disorders. While minimal side effects occur, it is important to discuss potential risks with a health care provider before starting treatment. Insurance companies and insurance providers may cover TMS therapy as an option for depression, making it more accessible for those seeking an alternative to invasive procedures. For potential patients considering TMS, consulting a treatment team can help determine the best treatment plan for brain health and normal activities. Seeking Treatment? We Can Help! At Sullivan Recovery, as an in-network provider we work with most insurance plans, such as: Tricare Blue Shield
Cymbalta Ruined My Life: Understanding the Risks and Recovery Options
Table of Contents Seeking Drug Or Alcohol Detox? Sullivan Recovery is a leading drug and alcohol detox in Mission Viejo, California. Call Today! Clinically Reviewed By: Rachel Sweet | LMFT Cymbalta Ruined My Life: Understanding the Risks and Recovery Options Understanding Cymbalta: An Overview Cymbalta (duloxetine) is a serotonin-norepinephrine reuptake inhibitor (SNRI) used to treat major depression, generalized anxiety disorder, and chronic pain conditions such as musculoskeletal pain and neuropathic pain. While it is considered an effective medication, some individuals experience negative effects, long-term side effects, and severe withdrawal symptoms that impact their daily lives. Mechanism of Action: How Cymbalta Works Effect on Brain Chemistry Cymbalta alters brain chemistry by increasing serotonin levels and norepinephrine levels, neurotransmitters responsible for mood regulation and pain perception. This action can improve symptoms of depression and anxiety symptoms but may also lead to emotional blunting, mood swings, and psychological symptoms such as brain fog and lack of energy. Physical Effects on the Body Cymbalta impacts various systems, including blood pressure, heart rate, and liver function. Some people experience rapid heartbeat, shortness of breath, gastrointestinal bleeding, and orthostatic hypotension (a sudden drop in blood pressure upon standing). Long-term use has been linked to liver damage, especially in individuals with a liver condition or those using recreational drugs or blood thinners. Indications for Use: Why Cymbalta is Prescribed Treatment for Depressive Disorder Cymbalta is FDA-approved for treating major depression and severe depression by regulating the reuptake of serotonin and norepinephrine after reliance on the medication. However, long-term Cymbalta use may result in addictive properties and uncomfortable withdrawal symptoms when discontinuing the drug. Managing Generalized Anxiety Disorder Healthcare professionals prescribe Cymbalta for generalized anxiety disorder (GAD) to help control excessive worry and panic attacks. However, some patients experience vivid dreams, sleep disturbances, and emotional instability as common side effects. Addressing Chronic Pain Conditions Cymbalta helps manage nerve pain, joint pain, and other types of pain by altering the body’s pain response. However, long-term side effects may include muscle aches, muscle spasms, and severe symptoms such as loss of consciousness or blood in urine. Side Effects of Cymbalta: What to Expect Common Side Effects Nausea Drowsiness Dry mouth Dizziness Sleep disturbances Weight gain or weight loss Severe Side Effects Suicidal ideation Serotonin syndrome Sexual dysfunction and loss of sexual desire Liver failure and drug-induced liver injury Severe withdrawal effects The Dark Side: Personal Accounts of Adverse Effects Emotional and Psychological Struggles Many individuals report mood swings, emotional blunting, and lack of mental balance while taking Cymbalta. Some describe feeling disconnected from their emotions, leading to psychiatric medication dependency and behavioral health issues. Physical Health Challenges Negative side effects include chronic fatigue, high blood pressure, rapid heartbeat, and pain signals becoming more intense over time. Patients also report abdominal bleeding and gastrointestinal bleeding as potential risks. Withdrawal Symptoms: The Transition Off Cymbalta Understanding Withdrawal Stopping Cymbalta suddenly can lead to severe withdrawal symptoms, including flu-like symptoms, brain zaps, unpleasant withdrawal symptoms, and common withdrawal symptoms like headaches, nausea, and anxiety symptoms. Coping with Discontinuation Syndrome To minimize withdrawal symptoms, a gradual tapering process under the supervision of a medical professional is recommended. A structured withdrawal process can help prevent severe withdrawal effects and unpleasant withdrawal symptoms. Potential for Addiction: Is Cymbalta Habit-Forming? Risk Factors for Dependence Although not classified as an addictive drug, Cymbalta can lead to psychological symptoms and dependency signs, making it difficult to stop using. Recognizing Dependency Signs Inability to function without Cymbalta Intensified symptoms of depression when missing a dose Needing higher doses for the same effect Precautions When Taking Cymbalta Medical Considerations Before starting Cymbalta, discuss any medical conditions with a healthcare provider, especially those involving blood pressure, liver condition, bipolar disorder, or chronic pain conditions. Interaction with Other Medications Cymbalta may interact with blood thinners, tricyclic antidepressants, alternative medications, and pain medications, leading to adverse effects. Coping Strategies for Those Affected by Cymbalta Mental Health Support If you struggle with mental health issues due to long-term Cymbalta use, specialized outpatient treatment programs at Sullivan Recovery can help you regain control of your mental health. Lifestyle Adjustments and Self-Care Maintaining a healthy lifestyle with a balanced diet, adequate sleep, physical activity, and stress management techniques such as salt baths, fish oil supplements, and non-pharmacological therapies can improve well-being. Support Groups and Resources Connecting with others facing similar struggles can offer emotional support and guidance through the withdrawal process. Exploring Alternative Treatments Non-Pharmacological Options Therapies like cognitive-behavioral therapy (CBT), alternative therapies, and holistic recovery approaches can help manage symptoms of depression and anxiety symptoms without medication. Other Medications for Mental Health and Pain For those who cannot tolerate Cymbalta, alternative antidepressant drugs may be available. Consulting a healthcare provider about alternative medications can help find a safer solution. Conclusion: Understanding Your Relationship with Cymbalta Cymbalta can be beneficial for some but has led to adverse side effects and negative effects for many others. If you are struggling with long-term Cymbalta use, withdrawal symptoms, or addiction treatment programs, Sullivan Recovery offers personalized treatment plans to support your recovery. Taking a courageous step toward healing is possible. Contact Sullivan Recovery today to begin your journey toward a healthier future. Seeking Treatment? We Can Help! At Sullivan Recovery, as an in-network provider we work with most insurance plans, such as: Tricare Blue Shield Magellan Health First Health Network The Holman Group Cigna Anthem BCBS Aetna Humana TriWest HMC Healthworks Molina UnitedHealthcare Optum UMR And More If you or a loved one are struggling with mental health challenges or substance abuse, reach out to Sullivan Recovery today. Our team of compassionate professionals is here to support your journey towards lasting well-being. Give us a call at 949-836-7180. Frequently Asked Questions 1. What are the most common side effects of Cymbalta? Cymbalta can cause common side effects such as nausea, dizziness, dry mouth, drowsiness, weight gain or weight loss, and sleep disturbances. Some individuals may also experience brain fog, emotional blunting, sexual dysfunction, and increased anxiety symptoms. In some cases, Cymbalta can lead
K18 Pill: Uses, Risks, and Treatment Options

Table of Contents Seeking Drug Or Alcohol Detox? Sullivan Recovery is a leading drug and alcohol detox in Mission Viejo, California. Call Today! Clinically Reviewed By: Rachel Sweet | LMFT K18 Pill: Uses, Risks, and Treatment Options The K18 pill is a prescription drug used for effective pain management. It contains oxycodone hydrochloride, an opioid pain medication prescribed to relieve severe pain. As a powerful opioid, it has a potential for abuse and a risk of addiction when misused. Understanding its uses, dosage, potential side effects, and treatment options is essential for patient safety. What Is the K18 Pill? The K18 pill is a small, blue, round tablet with an imprint of “K18.” It contains oxycodone hydrochloride 5 mg, an immediate-release oxycodone formulation. This opioid drug is used to treat acute pain, injury-related pain, and postoperative pain, as well as cancer-related pain in some cases. Medical professionals prescribe it under careful monitoring to minimize the risk of overdose and opioid use disorder. Uses of the K18 Pill Pain Management The pain-relieving effects of oxycodone hydrochloride tablets work by binding to mu-opioid receptors in the brain and spinal cord, altering the perception of pain. These opioid medications help patients with chronic ailments such as chronic pain conditions, postoperative pain, and cancer-related pain. Off-Label Uses While the oxycodone hydrochloride tablet is primarily used for pain relief, some healthcare providers may prescribe it for alternative treatment options in select cases. However, off-label use should only be under the supervision of a healthcare professional to prevent opioid addiction and other adverse effects. Dosage Guidelines Recommended Dosage The usual dose of oxycodone hydrochloride for acute pain is 5 mg every 4 to 6 hours as needed. Patients should always take the prescribed dose as directed by their healthcare provider to avoid the risk of dependence and fatal overdose. Adjustments for Specific Populations Elderly patients may require dosage adjustments due to changes in renal function and adrenal function. Patients with compromised liver or kidney function need a dose adjustment to reduce the risk of concentration of oxycodone in the bloodstream. Those with opioid tolerance may require an individualized treatment plan with an extended-release oxycodone formulation. Side Effects Common Side Effects Nausea Dizziness Abdominal pain Chest pain Constipation Short-term side effects like dry mouth Severe Side Effects Respiratory depression Life-threatening respiratory depression Clammy skin Trouble breathing Allergic reactions such as skin reactions Potential for Addiction Oxycodone pills have a high potential for addiction, especially with long-term use. Signs of addiction include: Increased physical dependence Seeking multiple prescriptions (doctor shopping) Experiencing withdrawal symptoms such as anxiety, nausea, and sweating Declining quality of life due to compulsive use Effects on the Brain and Body Mechanism of Action The action of oxycodone involves binding to opioid receptors in the central nervous system, altering pain signals and causing analgesic effects. However, long-term use can lead to opioid withdrawal syndrome and depression secondary to drug dependence. Impact on Mood and Behavior Prolonged use of opioid medications can affect cognitive function and emotional regulation, leading to depression, anxiety, and impaired decision-making. Interactions with Other Substances Alcohol and Other Drugs Mixing oxycodone hydrochloride with alcohol, depressant drugs, or nervous system depressants can lead to breathing difficulties, accidental overdose, and fatal overdose. Role of Prescribed Medications Certain prescription medications such as anticholinergic drugs, opioid receptor antagonists, and alternative treatments can interact with oxycodone, requiring a careful patient treatment goals assessment. Risks of Misuse Overdose Risks An overdose of oxycodone can cause circulatory depression, intracranial pressure, and even paralytic ileus. Symptoms include: Slow or stopped breathing Pinpoint pupils Unconsciousness Long-Term Health Implications Chronic opioid use can lead to dependence to oxycodone, opioid use disorder, and an increased risk of overdose. Prolonged exposure alters oxycodone plasma concentration, affecting the body’s stable drug effects. Treatment Options for K18 Pill Misuse Rehabilitation Programs Addiction treatment centers offer individualized treatment plans, including behavioral therapy, medical detox, and alternative treatment options. Programs such as the Transcend Recovery Community provide structured recovery support. Support Groups and Counseling Family therapy helps patients address family history of substance abuse. Group counseling supports patients through their journey to recovery. Cognitive-behavioral therapy (CBT) aids in managing addiction triggers. Conclusion The K18 pills containing oxycodone hydrochloride are an effective opioid pain medication but come with serious potential risks. Medical professionals must carefully monitor patients to prevent opioid addiction, pill addiction, and prescription drug abuse. Safe use requires adherence to the prescribed dose, avoiding illicit drugs, and considering alternative treatment options. If you or someone you know is struggling with substance use disorder, seek help from a healthcare provider or an addiction treatment center to start the path to recovery. Seeking Treatment? We Can Help! At Sullivan Recovery, as an in-network provider we work with most insurance plans, such as: Tricare Blue Shield Magellan Health First Health Network The Holman Group Cigna Anthem BCBS Aetna Humana TriWest HMC Healthworks Molina UnitedHealthcare Optum UMR And More If you or a loved one are struggling with mental health challenges or substance abuse, reach out to Sullivan Recovery today. Our team of compassionate professionals is here to support your journey towards lasting well-being. Give us a call at 949-836-7180. Frequently Asked Questions 1. What is the K18 pill used for? The K18 pill contains oxycodone hydrochloride 5 mg, an opioid pain medication prescribed for moderate to severe pain. It is commonly used for postoperative pain, injury-related pain, and chronic pain conditions. Due to its potential for addiction and dependence, it should only be taken as prescribed by a healthcare provider. 2. What are the risks of taking the K18 pill? The K18 pill carries several potential risks, including opioid addiction, physical dependence, and respiratory depression. Misuse or overdose can lead to life-threatening respiratory depression, circulatory depression, and fatal overdose. Patients should also be aware of common side effects such as dizziness, nausea, and constipation, as well as severe side effects like trouble breathing and chest pain. 3. Can the K18 pill interact with other medications or substances? Yes, the K18 pill can have dangerous
M367 Pill: Uses, Risks, and Safety Guidelines

Table of Contents Seeking Drug Or Alcohol Detox? Sullivan Recovery is a leading drug and alcohol detox in Mission Viejo, California. Call Today! Clinically Reviewed By: Rachel Sweet | LMFT M367 Pill: Uses, Risks, and Safety Guidelines What Is the M367 Pill? The M367 pill is a prescription opioid pain medication used for effective pain relief in patients suffering from severe pain. This combination medication contains hydrocodone and acetaminophen, both of which work together to alleviate pain signals sent through the Central Nervous System. As an opioid analgesic, M367 pills interact with opioid receptors in the brain and spinal cord to reduce discomfort. Due to its opioid content, it carries a potential risk for opioid addiction, physical dependence, and psychological dependence. M367 pills are manufactured by Mallinckrodt Pharmaceuticals and are available in tablet form with an imprint code that helps in identification. Appearance and Identification M367 pills are oval pills that are white in color and have M367 imprinted on one side. The active ingredients in each pill include 10 mg of hydrocodone bitartrate and 325 mg of acetaminophen. These acetaminophen tablets are formulated with inactive ingredients like magnesium stearate, microcrystalline cellulose, and silicon dioxide to maintain the structure and stability of the pill. Mallinckrodt Inc. ensures that these prescription medications meet adequate studies and clinical studies for patient safety. Medical Uses of M367 M367 is commonly prescribed for chronic pain conditions, post-surgical pain, and other cases requiring short-term use of a prescription opioid pain medication. The opioid component in M367 provides a degree of analgesia by interacting with opioid receptors, while the acetaminophen component enhances its effectiveness. However, long-term use can increase the risk of dependence and development of tolerance varies from person to person. Potential Risks and Side Effects Common Side Effects M367 pills can cause mild to severe side effects, including drowsiness, dizziness, nausea, constipation, mental clouding, urinary retention, and hearing impairment. These effects are common with opioid drugs and should be monitored under medical supervision. Severe Side Effects and Overdose Risks In higher doses, M367 can cause dose-related respiratory depression, leading to shallow breathing, respiratory rhythm abnormalities, and cardiovascular depression. Symptoms of an overdose with hydrocodone may include clammy skin, extreme somnolence, circulatory collapse, and cardiac arrest. Acetaminophen overdosage can lead to liver injury, liver metabolism dysfunction, and risk of liver damage, particularly in patients with pre-existing liver conditions. Toxic doses of acetaminophen can cause abdominal pain, hepatotoxic overdose, and failure of liver function. In cases of acute overdosage, emergency medical attention is necessary. Contact a regional poison control center or Poison Control System immediately. Addiction and Abuse Potential The opioid crisis has highlighted the potential for addiction in opioid medications like M367. The effects of hydrocodone can create feelings of euphoria, leading to misuse and dependency. Opioid use disorder can develop with long-term use, and sensitive patients such as elderly patients or patients with head injuries are at an even higher risk. Behavioral therapies and medication-assisted treatments are available for those experiencing opioid addiction. Dangers of Counterfeit Pills The circulation of counterfeit pills poses a significant health risk, as they may contain lethal polydrug overdose substances like fentanyl. These counterfeit tablets often have an identical pill form but lack proper dosing range regulations, increasing the risk of overdose. Patients should only obtain prescription opioid pain medication from licensed healthcare providers to avoid counter medications that may contain hazardous substances. Dosage Guidelines M367 pills should be taken via oral administration, following a dose selection based on the patient’s needs. The standard oral dose is one tablet every 4 to 6 hours as needed for pain relief. Patients should not exceed 4,000 mg of acetaminophen per day, as this increases the risk of acetaminophen overdose. Hypersensitivity to hydrocodone may occur in some individuals, requiring an adjustment in treatment. Therapeutic doses should be strictly monitored by a medical professional. Treatment Options for Dependence For individuals experiencing opioid addiction, treatment involves behavioral therapies, medication-assisted treatments, and long-term recovery programs. MAT options such as buprenorphine and methadone help reduce withdrawal symptoms and psychic dependence. Rehabilitation centers and drug therapy programs provide support in the journey to recovery. DEA Classification and Legal Implications M367 is classified as a Schedule II controlled substance, indicating a high potential for addiction and abuse. Possession without a prescription from a healthcare provider can lead to legal consequences, including fines and imprisonment. Laws surrounding prescription opioid pain medication aim to combat the opioid epidemic and prevent adverse drug events caused by misuse. The Opioid Epidemic and M367 The opioid crisis continues to be a major concern, with prescription medications like M367 contributing to accidental ingestion, opioid overdose, and development of addiction. Reports indicate that the opioid epidemic has led to an increase in emergency medical visits, lethal overdoses, and a strain on public health resources. The existence of opiate receptors in the body contributes to opioid addiction, making prevention and education efforts crucial. Best Practices for Safe Usage Patients should follow medical supervision when using M367 to prevent potential side effects and health risks. Monitoring liver function, renal function tests, and cardiorespiratory function is essential for debilitated patients or those with concomitant disease. Avoid mixing M367 with nervous system depressants such as alcohol or antianxiety agents, as this can lead to adverse effects on therapy. Seeking Professional Help For individuals struggling with opioid use disorder, seeking help early can prevent severe consequences. Healthcare professionals and opioid addiction specialists can provide guidance on long-term recovery. Rehabilitation centers, therapy programs, and opioid antagonists like naloxone (Narcan) are available for emergency intervention. If you or someone you know is struggling, contact SAMHSA’s National Helpline (1-800-662-HELP) or a local addiction treatment center. Conclusion M367 pills provide effective pain relief but come with significant risks. Proper medical attention, healthcare provider guidance, and adherence to prescribed dosages are essential for safe use. The opioid epidemic has made it critical to recognize the potential risks of opioid pain relievers and seek help when needed. If dependence develops, a structured recovery journey with
Narcotics Anonymous (NA): A Comprehensive Guide to the 12 Steps and Recovery

Table of Contents Seeking Drug Or Alcohol Detox? Sullivan Recovery is a leading drug and alcohol detox in Mission Viejo, California. Call Today! Clinically Reviewed By: Rachel Sweet | LMFT Narcotics Anonymous (NA): A Comprehensive Guide to the 12 NA Steps and Recovery What is Narcotics Anonymous (NA)? Narcotics Anonymous (NA) is a nonprofit fellowship designed to help individuals struggling with substance use disorders, including addiction to drugs and prescription drugs. As an independent organization, NA provides a safe and confidential space for people in recovery to explore their challenges, share experiences, and find a path to recovery. The Origins of NA NA was founded in 1953 as a sister organization to Alcoholics Anonymous (AA). While AA focuses on alcohol abuse and alcohol use disorder, NA extends support to those recovering from a wide range of addiction types, including drug abuse and addiction beyond alcohol. NA’s foundation rests on the 12-Step recovery model, emphasizing complete abstinence and spiritual principles. Goals and Principles of NA The goals of NA are to help individuals achieve recovery from addiction and build a better daily life free from the cycle of substance abuse. Core principles include honesty, accountability, and a commitment to personal growth. NA also focuses on helping members uncover underlying issues contributing to their addiction. Understanding the 12 Steps of NA The 12-Step philosophy is central to the NA recovery program. These steps guide individuals in recovery through self-awareness, accountability, and spiritual growth, fostering their journey to recovery. Step 1: Admitting Powerlessness Individuals recognize their active addiction and acknowledge they cannot overcome it alone. Step 2: Believing in a Higher Power Participants explore the concept of a higher power, which can be interpreted personally, fostering a sense of hope. Step 3: Making a Decision to Turn Over Control This step emphasizes trust in the higher power and the willingness to embrace change. Step 4: Conducting a Moral Inventory Through self-reflection, participants examine their actions and behaviors to create a personal inventory of their defects of character. Step 5: Admitting Wrongdoing This step involves sharing one’s moral inventory with another person, promoting conscious contact with a higher power. Step 6: Ready for Higher Power to Remove Shortcomings Participants become open to change, allowing their higher power to help with character defects. Step 7: Asking for Humility This step emphasizes humility and actively seeking help in overcoming shortcomings. Step 8: Listing Those Harmed Individuals list people they have hurt during their battle with substance abuse, paving the way for amends. Step 9: Making Amends By taking direct action, participants repair their record with relationships, fostering healing for both parties. Step 10: Continuing Personal Inventory Participants maintain regular attendance in meetings and self-assess to prevent relapse and address new challenges. Step 11: Seeking Spiritual Connection This step emphasizes maintaining conscious contact with a higher power for ongoing spiritual growth. Step 12: Carrying the Message to Others Participants help others struggling with addiction by sharing their personal experiences and spreading the message to addicts still suffering. Structure of NA Meetings NA meetings provide a safe space for individuals in recovery to connect. Meetings are held in community centers, treatment programs, and even through online meetings or virtual meetings for accessibility. There are Closed meetings, restricted to individuals in recovery, and Open meetings, welcoming anyone interested in learning about NA. What Newcomers Can Expect in NA Meetings Newcomers can expect a welcoming environment and the opportunity to observe or share as they feel comfortable. They’ll be introduced to 12-Step literature and encouraged to explore 12-Step participation through 12-Step group involvement. Alternative Support Systems for Addiction While NA is widely accessible, other treatment options include inpatient treatment programs, outpatient substance abuse treatment, and behavioral therapy. These options complement the 12-Step methodology by addressing addiction’s mental and physical aspects. Importance of Community in Recovery The addiction recovery community plays a vital role in helping individuals navigate the addiction recovery journey. 12-Step fellowship offers members a confidential space to share, fostering a sense of belonging and accountability. The Role of Continuous Personal Inventory The 12-Step recovery model emphasizes the importance of ongoing self-reflection. This process allows individuals in treatment experiences to address character defects and maintain progress in recovery. Differences Between NA and Alcoholics Anonymous (AA) NA and AA share the 12-Step framework, but their focus differs. NA addresses a broader range of addiction, including drug abuse, while AA primarily focuses on recovery from alcohol addiction. Both programs promote spiritual awakening and core principles of accountability and growth. Tips for Seeking Help with Substance Use Contact a Treatment Center: Reach out to addiction care specialists for personalized guidance. Explore 12-Step Groups: Attend regular meetings in NA or similar twelve-step programs like Cocaine Anonymous. Use Online Resources: Tools like the online treatment locator or Mental Health Services Administration directory can help. Verify Insurance: Work with a healthcare provider to confirm insurance verification for treatment. Commit to Recovery: Engage in 12-Step service and other support options to strengthen recovery efforts. Accessibility and Spiritual Aspects of the 12-Step Model The 12-Step models, including NA, are accessible and inclusive, allowing members to interpret the concept of a higher power in a way that resonates with them. This flexibility fosters addiction mutual-help and self-help programs, empowering individuals to find spiritual awakening and personal growth. By embracing the principles of Narcotics Anonymous, individuals can break free from the disease of addiction, discover the path to complete abstinence, and embark on a lifelong journey to recovery. Seeking Treatment? We Can Help! At Sullivan Recovery, as an in-network provider we work with most insurance plans, such as: Tricare Blue Shield Magellan Health First Health Network The Holman Group Cigna Anthem BCBS Aetna Humana TriWest HMC Healthworks Molina UnitedHealthcare Optum UMR And More If you or a loved one are struggling with mental health challenges or substance abuse, reach out to Sullivan Recovery today. Our team of compassionate professionals is here to support your journey towards lasting well-being. Give us a call at 949-836-7180. Frequently Asked Questions 1. What is Narcotics Anonymous
Understanding the AA Preamble: A Roadmap to Recovery
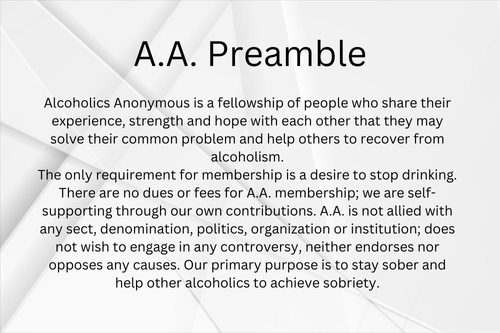
Table of Contents Seeking Drug Or Alcohol Detox? Sullivan Recovery is a leading drug and alcohol detox in Mission Viejo, California. Call Today! Clinically Reviewed By: Rachel Sweet | LMFT Understanding the AA Preamble: A Roadmap to Recovery The AA Preamble is a cornerstone of Alcoholics Anonymous (AA) and serves as a guiding framework for the fellowship of people working towards their journey to sobriety. This article delves into the significance, evolution, and core principles of the A.A. Preamble – 2024, showcasing how it fosters holistic recovery and supports countless individuals in their path to recovery from alcohol addiction. Significance of the AA Preamble The AA Preamble introduces the essence of Alcoholics Anonymous, outlining the criterion for membership: a genuine desire to stop drinking. It emphasizes the power of unity within the recovery community and highlights the importance of collective sharing and shared experiences in overcoming dependence on alcohol. Purpose and Goals of the AA Preamble The A.A. Preamble AA clearly defines the organization’s purpose: helping those seeking recovery from alcoholism achieve lasting sobriety. By promoting inclusive language, the Preamble creates a welcoming environment where stories of recovery resonate, and members are inspired to support one another in their recovery journey. Evolution of the AA Preamble Original Version (1940) Introduced in 1947, the original AA Preamble set the foundation for the AA program, establishing its mission and approach to helping people achieve a life of sobriety. Key Revisions Over the Years The Preamble’s language has been updated over time to reflect societal changes. These revisions ensure it remains relevant and inclusive, empowering individuals on their road to recovery. Core Principles of the AA Preamble Desire to Stop DrinkingThe only requirement for membership in AA is an honest desire to stop drinking. This commitment forms the basis of personal and transformative recovery experiences. Self-Supporting NatureAA does not rely on external funding or membership fees, maintaining its independence and neutrality. This self-sufficiency underscores the importance of individual contributions within the recovery community. Neutrality and IndependenceThe Preamble reinforces AA’s commitment to being free from political, religious, or institutional affiliations, ensuring focus on the journey towards sobriety and recovery from addiction. Integration of the AA Preamble in Recovery Treatments Role of Liberty Addiction Recovery in AA Philosophy At Liberty Addiction Recovery, the core values of the AA Preamble align with their recovery curriculum. By focusing on shared experiences and the transformative power of community, they create a roadmap to recovery for individuals. The AA Program in Recovery Communities The AA program plays a critical role in various treatment programs, fostering personal recovery and encouraging participation in annual meetings, where members strengthen their commitment to sobriety. The AA Preamble in Practice Real-Life Applications in AA Meetings Every AA meeting begins with a moment of silence, followed by the A.A. Preamble, setting a reflective tone for participants. These gatherings encourage collective sharing and allow members to navigate the barriers people face in recovery. Community Support and Fellowship The presence in recovery communities fosters long-term recovery through mutual support. By focusing on the pinnacle of sobriety, members build relationships based on trust and understanding. Common Misconceptions About the AA Preamble It’s Only for People in Recovery from AlcoholismWhile the Preamble focuses on alcohol dependence, its core principles resonate with individuals in all stages of recovery from addiction. It’s Just a Formality in MeetingsThe AA preamble is a vital element, reminding members of the shared commitment to recovery and the transformative power of unity. FAQs on the AA Preamble What is the AA Preamble? The AA Preamble is a concise introduction to Alcoholic Anonymous that defines its mission, principles, and goal of recovery. Why is the AA Preamble important for recovery? It provides a clear structure, emphasizing shared experiences and the collective journey of people in recovery. How has the AA Preamble influenced other recovery programs? The Preamble has shaped many recovery programs, inspiring inclusivity, independence, and a commitment to the journey of recovery. Conclusion and Key Takeaways The AA Preamble is a beacon for those seeking freedom from alcohol addiction. Its focus on the 12-step program, personal recovery, and the transformative power of community creates a solid foundation for individuals on their road to recovery. For those starting their journey to sobriety, the AA Preamble serves as a reminder of the power of unity and the potential for a dual-faceted recovery: overcoming alcohol dependence while embracing a fulfilling life of sobriety. Further Resources for Understanding the AA Preamble Explore the Chat FAQ Meeting Schedule Service for upcoming AA meeting times. Connect with local AA groups to experience the AA preamble in action. Visit Liberty Addiction Recovery for information on integrating AA principles into your treatment program. Let the AA Preamble guide you on your journey to recovery, empowering you to embrace a brighter, sober future. Seeking Treatment? We Can Help! At Sullivan Recovery, as an in-network provider we work with most insurance plans, such as: Tricare Blue Shield Magellan Health First Health Network The Holman Group Cigna Anthem BCBS Aetna Humana TriWest HMC Healthworks Molina UnitedHealthcare Optum UMR And More If you or a loved one are struggling with mental health challenges or substance abuse, reach out to Sullivan Recovery today. Our team of compassionate professionals is here to support your journey towards lasting well-being. Give us a call at 949-836-7180. Frequently Asked Questions 1. What is the purpose of the A.A. Preamble? The A.A. Preamble introduces the mission and principles of Alcoholics Anonymous. It serves as a welcoming statement, fostering unity and emphasizing the shared goal of sobriety. By highlighting the requirement for membership—an honest desire to stop drinking—it ensures inclusivity and clarity for anyone seeking help. 2. Why is the A.A. Preamble read at meetings? The A.A. Preamble sets the tone for every A.A. meeting, reminding attendees of the core principles and values that guide the fellowship. It reinforces the importance of mutual support, neutrality, and the commitment to helping one another on the journey to recovery. Starting meetings with the Preamble creates a sense of focus and
Why Is Cocaine Addictive? A Deep Dive into Its Chemistry
Table of Contents Seeking Drug Or Alcohol Detox? Sullivan Recovery is a leading drug and alcohol detox in Mission Viejo, California. Call Today! Clinically Reviewed By: Rachel Sweet | LMFT Why Is Cocaine Addictive? A Deep Dive into Its Chemistry Cocaine is a powerful stimulant that affects the brain in profound ways. Its addictive potential stems from its biochemical effects, interactions with the brain’s reward system, and the psychological and societal factors surrounding its use. Understanding why cocaine is addictive can shed light on the challenges of overcoming this substance. The Biochemical Effects of Cocaine Cocaine alters brain chemistry, primarily by interfering with dopamine, a neurotransmitter linked to pleasure and reward. This interference produces intense feelings of euphoria, but it also disrupts the brain’s natural balance. How Cocaine Interacts with Dopamine Cocaine blocks the dopamine transporter, leading to a buildup of this neurotransmitter in the brain’s synapses. This flood of dopamine enhances feelings of euphoria, creating a powerful incentive to use the drug repeatedly. The release of dopamine contributes to the addictive potential of cocaine. The Role of the Brain’s Reward System The brain’s reward pathway reinforces behaviors that provide pleasure or are essential for survival. Cocaine acts on the nucleus accumbens and dopaminergic cells, hijacking this system and making the brain associate its use with an essential need. Over time, natural rewards become less satisfying, increasing reliance on the drug. The Onset and Duration of Cocaine Effects The effects of cocaine set in rapidly and fade quickly, contributing to its addictive nature. Rapid Onset of Euphoria When snorted, smoked, or injected, cocaine’s effects can be felt within seconds. This quick onset creates an immediate positive reinforcement loop, making users crave the drug almost instantly. The euphoric effects of cocaine can be attributed to the excessive dopamine activity resulting from its use. Short Duration of High The euphoric effects of cocaine, or feelings of euphoria, are short-lived, often lasting only 15 to 30 minutes. This brevity encourages frequent doses to maintain the high, leading to a cycle of addiction and increased risk of overdose. Tolerance and Increased Usage Cocaine’s addictive potential increases with tolerance, a phenomenon where the body requires higher doses to achieve the same effects. Understanding Drug Tolerance As the brain adapts to cocaine, it becomes less responsive to the drug’s effects. Users then consume larger doses to feel the same euphoria, escalating the risk of addiction. Chronic cocaine exposure exacerbates this process, leading to eventual cocaine dependence. Compounding Effects of Repeated Use Frequent use intensifies cocaine’s impact on the brain, causing more profound chemical imbalances. This leads to stronger cravings for cocaine and an increased likelihood of compulsive drug-seeking behavior. Cocaine users often experience withdrawal symptoms, including intense cravings and physical dependence. Mixing Cocaine with Other Substances Combining cocaine with other substances exacerbates its addictive properties and increases the risk of severe health consequences. The Dangers of Polydrug Use Mixing cocaine with alcohol, opioids, or other illegal drugs amplifies their combined effects. This can lead to dangerous outcomes, including overdose and long-term damage to the brain and body. Cocaine abusers engaging in polydrug use face heightened cardiovascular risks, including blood pressure spikes and heart attack. How Mixing Increases Addictiveness Polydrug use can intensify cravings and dependency by creating more complex interactions in the brain’s reward center. Cocaine use behavior often involves combining the drug with others, increasing the prevalence of cocaine use disorders and the difficulty of treatment. Psychological Factors in Cocaine Addiction Psychological influences also play a critical role in cocaine addiction, from mental health issues to societal pressures. Positive Reinforcement and Reward Cocaine creates a powerful association between its use and pleasure. This positive reinforcement makes quitting especially challenging, as the brain continually seeks the reward it associates with the drug. The cycle of cocaine addiction is reinforced by behavioral effects tied to the neurotransmitter dopamine. The Role of Mental Health Disorders Conditions like anxiety, depression, bipolar disorder, and PTSD can increase susceptibility to cocaine addiction. Many individuals turn to cocaine as a coping mechanism, further entrenching its use and leading to substance use disorder. The psychological dependence on cocaine is often accompanied by physical symptoms of addiction. Societal Influences on Cocaine Use Cultural and social factors shape attitudes toward cocaine use and affect its prevalence in certain communities. Cultural Attitudes Towards Cocaine In some circles, cocaine is glamorized as a symbol of success or sophistication. This perception can encourage experimentation and normalize its use. Recreational drug use, including first-time cocaine use, is often influenced by peer pressure and societal norms. Socioeconomic Status and Availability Cocaine’s availability and cost vary by region and socioeconomic status. In areas where the drug is more accessible, addiction rates tend to be higher. Exposure to cocaine is more common in environments where substance abuse disorder is prevalent, further driving the cycle of abuse. Conclusion Cocaine addiction is driven by a combination of biochemical effects, psychological factors, and societal influences. Its impact on the brain’s reward system, combined with the rapid onset and short duration of its effects, makes it highly addictive. The harmful effects of cocaine use include withdrawal symptoms, tolerance, and long-term damage to the brain and body. Understanding these factors highlights the importance of comprehensive treatment approaches, such as cognitive-behavioral therapy and behavioral therapies, to address both the physical and psychological aspects of addiction. At Sullivan Recovery, our cocaine addiction treatment program provides effective treatment and support for those seeking long-term recovery. We address the physiological effects and psychological consequences of addiction, offering a therapeutic approach that fosters healing and recovery. Seeking Treatment? We Can Help! At Sullivan Recovery, as an in-network provider we work with most insurance plans, such as: Tricare Blue Shield Magellan Health First Health Network The Holman Group Cigna Anthem BCBS Aetna Humana TriWest HMC Healthworks Molina UnitedHealthcare Optum UMR And More If you or a loved one are struggling with mental health challenges or substance abuse, reach out to Sullivan Recovery today. Our team of compassionate professionals is here to support your journey towards lasting
Quitting Alcohol Cold Turkey: Risks, Symptoms, and Safer Alternatives

Table of Contents Seeking Drug Or Alcohol Detox? Sullivan Recovery is a leading drug and alcohol detox in Mission Viejo, California. Call Today! Clinically Reviewed By: Rachel Sweet | LMFT Quitting Alcohol Cold Turkey: Risks, Symptoms, and Safer Alternatives Quitting alcohol cold turkey may seem like a quick solution, but it carries significant health risks, especially for individuals with severe alcohol dependence or alcohol use disorder. The process can lead to severe withdrawal symptoms and dangerous complications. Understanding the withdrawal process, exploring safer methods like a medical detox, and seeking professional care can improve outcomes and support long-term recovery. Risks of Quitting Alcohol Cold Turkey Severe Withdrawal Symptoms Abrupt cessation of alcohol intake can lead to a form of alcohol withdrawal known as alcohol withdrawal syndrome (AWS). This condition includes severe withdrawal symptoms such as nausea, vomiting, tremors, and excessive sweating. For individuals with severe alcohol dependence or a history of alcohol withdrawal, these symptoms can escalate rapidly. Life-Threatening Complications Quitting alcohol suddenly can result in delirium tremens, a severe form of alcohol withdrawal that includes confusion, rapid heart rate, and seizures. These dangerous symptoms can lead to fatal complications without immediate medical care. Heavy drinking over a long period increases the risk of severe alcohol withdrawal symptoms and complications like heart palpitations and even heart attack. Psychological Implications Withdrawal from alcohol not only impacts physical health but also affects mental health. Alcohol cravings, panic attacks, and worsening depression are common symptoms. These psychological effects often accompany intense withdrawal symptoms, making professional support essential during this period. Alcohol Withdrawal Timeline Initial Symptoms Common alcohol withdrawal symptoms typically appear within 6–12 hours after the last drink of alcohol. These symptoms include clammy skin, headaches, loss of appetite, and a rapid heart rate. Peak Symptoms The peak occurs within 24–72 hours, during which severe alcohol withdrawal symptoms like profuse sweating, severe confusion, and hallucinations manifest. This is the most critical phase of the withdrawal process, requiring close monitoring by healthcare professionals. Duration of Withdrawal Effects For most individuals, physical withdrawal symptoms subside within 5–7 days. However, post-acute withdrawal syndrome (PAWS) can prolong psychological symptoms like anxiety and alcohol cravings for weeks or months. Common Symptoms of Alcohol Withdrawal Physical Symptoms Excessive sweating Stomach pains Increased heart rate Muscle tremors Psychological Symptoms Intense cravings for alcohol Panic attacks Irritability and depression Difficulty concentrating Long-Term Effects of Alcohol Use Prolonged or excessive alcohol consumption can lead to significant health problems, including Wernicke-Korsakoff syndrome, liver damage, and neurological conditions. Even after achieving abstinence from alcohol, individuals must address the negative effects on both physical and mental health through ongoing treatment. Factors Affecting Withdrawal Duration and Amount of Alcohol Consumption Chronic alcohol misuse or drinking large amounts of alcohol per week significantly increases the severity of symptoms during withdrawal. Individual Health Conditions Underlying medical conditions, such as diabetes or cardiovascular issues, can complicate the management of alcohol withdrawal and elevate the risk of severe symptoms. Previous Withdrawal Experiences Individuals with a history of alcohol withdrawal are more likely to experience severe symptoms, including severe complications like seizures or alcohol withdrawal delirium. The Case for Medical Detox Importance of Professional Support A medical detox program offers a controlled environment where symptoms of withdrawal can be safely managed by healthcare professionals. Safe Management of Withdrawal Symptoms In a professional detox setting, prescription medications like benzodiazepines are used to reduce dangerous withdrawal symptoms and prevent life-threatening conditions. Monitoring Mental Health During Detox Comprehensive care includes addressing co-occurring mental health disorders such as anxiety, depression, and PTSD, which often accompany dependence on alcohol. Tapering Strategy as an Alternative Definition of Tapering Tapering involves reducing alcohol intake gradually to minimize physical withdrawal symptoms and prevent severe alcohol withdrawal. Benefits of Tapering Safer reduction of alcohol content in the body Lower risk of intense withdrawal symptoms Better preparation for complete abstinence from alcohol Implementation of a Tapering Schedule A successful taper requires professional guidance to monitor the withdrawal process and avoid potential dangers like severe symptoms or relapse. Seeking Professional Help Types of Addiction Treatment Programs Inpatient setting: Offers round-the-clock care in a supportive environment. Intensive outpatient program: Provides flexibility with structured care. Behavioral therapy: Focuses on managing cravings and addressing the root causes of addiction to alcohol. Importance of Comprehensive Care Effective recovery programs integrate medical care, therapy, and support groups like Alcoholics Anonymous to ensure long-term success. Resources for Finding Help Organizations such as the Substance Abuse and Mental Health Services Administration (SAMHSA) and American Addiction Centers provide valuable tools for finding treatment options. Quitting alcohol cold turkey puts your health at significant risk, especially for individuals with severe alcohol dependence. Exploring safer alternatives like medical detox or a tapering strategy, under the care of addiction specialists like Sullivan Recovery, can ensure a successful recovery process. Whether through inpatient care, outpatient programs, or support groups, recovery from alcohol addiction is an ongoing process that benefits from professional support and comprehensive care. Seeking Treatment? We Can Help! At Sullivan Recovery, as an in-network provider we work with most insurance plans, such as: Tricare Blue Shield Magellan Health First Health Network The Holman Group Cigna Anthem BCBS Aetna Humana TriWest HMC Healthworks Molina UnitedHealthcare Optum UMR And More If you or a loved one are struggling with mental health challenges or substance abuse, reach out to Sullivan Recovery today. Our team of compassionate professionals is here to support your journey towards lasting well-being. Give us a call at 949-836-7180. Frequently Asked Questions 1. What are the risks of quitting alcohol cold turkey? Quitting alcohol cold turkey can lead to serious health risks, especially for individuals with severe alcohol dependence or a long history of heavy drinking. The abrupt cessation of alcohol can trigger severe withdrawal symptoms such as tremors, nausea, and rapid heart rate. More dangerous symptoms, like seizures and delirium tremens (DTs), may develop, posing life-threatening risks. Psychological effects, including anxiety, depression, and intense alcohol cravings, can also occur. It is important to consult a medical professional to ensure a safe and effective withdrawal
Effexor Withdrawal: Essential Tips for Managing Symptoms and Recovery

Table of Contents Seeking Drug Or Alcohol Detox? Sullivan Recovery is a leading drug and alcohol detox in Mission Viejo, California. Call Today! Clinically Reviewed By: Rachel Sweet | LMFT Effexor Withdrawal: Essential Tips for Managing Symptoms and Recovery Effexor (venlafaxine) is an antidepressant medication that helps treat depression and anxiety disorders. While it is effective for managing mental health conditions, stopping Effexor abruptly can lead to severe withdrawal symptoms. This guide will cover Effexor withdrawal symptoms, the Effexor withdrawal timeline, and ways to manage the recovery process safely, including tapering off the medication. Understanding Antidepressant Discontinuation Syndrome Antidepressant discontinuation syndrome occurs when someone reduces or stops their medication too quickly, leading to uncomfortable discontinuation symptoms. These symptoms are common with SNRIs like Effexor due to its short half-life. Proper tapering, gradual reduction, and medical supervision are critical to managing this condition effectively. Effexor Withdrawal Symptoms Effexor withdrawal symptoms can include physical, psychological, and neurological effects: Physical symptoms: Nausea, flu-like symptoms, dizziness, and tingling sensations. Psychological symptoms: Mood swings, increased anxiety, and vivid dreams. Neurological symptoms: Brain zaps, electric shock-like sensations, and brain shivers. Common withdrawal symptoms like headaches and fatigue often improve with gradual tapering and a tapering schedule monitored by a healthcare provider. Effexor Withdrawal Timeline Initial Phase (Days 1-3) Withdrawal symptoms typically begin 24-48 hours after the last dose. Early signs include nausea, dizziness, headaches, and electric shock-like sensations. Peak Phase (Days 4-7) Symptoms like flu-like symptoms, mood swings, irritability, and vivid dreams usually intensify. Severe cases may involve suicidal thoughts or increased anxiety, making medical supervision essential. Recovery Process (Weeks 2 and Beyond) Most physical symptoms resolve by the second week, but psychological symptoms such as depression and anxiety may persist. This is when ongoing support, such as family therapy or support groups, becomes crucial. Building a strong support network can also be beneficial during this recovery phase. Managing Effexor Withdrawal At-Home Treatments Maintain regular sleep, proper hydration, and a balanced diet to support overall well-being. Engage in light exercise to reduce stress and boost serotonin levels. Practice stress management techniques like mindfulness and deep breathing. Professional Treatment Options Gradually reducing the dosage under a healthcare professional’s guidance with a structured tapering plan is the safest approach. Discuss the use of antihistamines or other antidepressants to manage severe symptoms. Coping with Withdrawal Coping with withdrawal from Effexor can be challenging, but there are several strategies that can help. Here are some tips to help you manage withdrawal symptoms: Take a Break Taking a break from work and other responsibilities can give you time to heal and recover from withdrawal symptoms. It’s essential to prioritize your health and well-being during this time. Consider taking a few days off work or reducing your workload to minimize stress and anxiety. This downtime allows your body and mind to adjust to the changes, making the withdrawal process more manageable. Stay Active Regular exercise can help boost your mood and reduce withdrawal symptoms. Engage in physical activities that you enjoy, such as walking, jogging, or yoga. Exercise can also help reduce stress and anxiety, which are common symptoms of withdrawal. Physical activity stimulates the release of endorphins, which can improve your overall sense of well-being and help counteract some of the discomfort associated with venlafaxine withdrawal. Reducing Withdrawal Symptoms Gradual Tapering Abruptly stopping Effexor increases the risk of severe symptoms, so a slow dose reduction over at least six weeks minimizes discomfort and ensures a smoother transition. Seek Professional Support A healthcare provider can create a customized taper plan based on your current dose and health needs. This reduces the likelihood of severe venlafaxine withdrawal symptoms through careful monitoring. Safety Precautions It’s essential to take safety precautions when withdrawing from Effexor to minimize the risk of severe withdrawal symptoms. Here are some tips to help you stay safe: Create a Safety Plan Create a safety plan with your healthcare provider to ensure you have support during the withdrawal process. This plan should include: A tapering schedule to gradually reduce your dosage, minimizing the risk of severe withdrawal symptoms. Regular check-ins with your healthcare provider to monitor your progress and adjust the plan as needed. A list of emergency contact numbers, such as your healthcare provider or a crisis hotline, in case you experience severe symptoms. A plan for managing severe withdrawal symptoms, such as brain zaps or suicidal thoughts, ensuring you have immediate access to help if needed. By following these safety precautions and coping strategies, you can minimize the risk of severe withdrawal symptoms and ensure a safe and successful withdrawal from Effexor. Remember, the support of a healthcare provider is crucial in navigating this challenging process, and taking proactive steps can make a significant difference in your recovery journey. FAQs How long does Effexor withdrawal last? The duration of venlafaxine withdrawal varies due to individual variability but typically lasts several weeks. Psychological symptoms like mood changes may take longer to subside. What do Effexor brain zaps feel like? Brain zaps are described as sudden, shock-like sensory disturbances in the brain, often triggered by abrupt discontinuation or missing a dose. How to taper off 75 mg Effexor? Work with a healthcare professional to slowly reduce the daily dose through careful dose adjustments, ensuring a safe withdrawal process. Conclusion Effexor withdrawal can be a daunting experience, but it’s important to remember that recovery is achievable with the right approach and support. A carefully planned tapering schedule, created and monitored by a trusted healthcare provider, is the most effective way to minimize withdrawal symptoms and ensure a safe transition off the medication. Avoid the temptation to stop Effexor suddenly, as abrupt discontinuation significantly increases the risk of severe withdrawal symptoms, including brain zaps, mood swings, and intense anxiety. Managing Effexor withdrawal requires both physical and emotional care. Focus on maintaining a healthy lifestyle by prioritizing regular sleep, proper nutrition, and physical activity. These simple actions can help your body cope with the changes while reducing the intensity of physical symptoms like
Top Signs Someone is on Meth: Recognizing the Symptoms Early

Table of Contents Seeking Drug Or Alcohol Detox? Sullivan Recovery is a leading drug and alcohol detox in Mission Viejo, California. Call Today! Clinically Reviewed By: Rachel Sweet | LMFT Top Signs Someone is on Meth: Recognizing the Symptoms Early Methamphetamine, often referred to as crystal meth, is a highly addictive drug that directly impacts the central nervous system. Classified as a Schedule II controlled substance by the Drug Enforcement Administration (DEA), methamphetamine has a high potential for misuse, dependence, and devastating health consequences. Early identification of the signs someone is on meth is critical for preventing long-term health problems and offering timely intervention. This article provides an in-depth look at the physical symptoms, behavioral changes, and risks associated with meth use, while highlighting effective meth addiction treatment options. Understanding Methamphetamine Abuse Methamphetamine abuse leads to profound changes in brain chemistry, which can result in mental health conditions like anxiety, depression, and psychosis. Prolonged abuse of this stimulant drug affects every aspect of a person’s life, from their physical health to their relationships and daily functioning. Substance abuse of meth often leads to erratic behavior, mood instability, and neglect of responsibilities. Without intervention, the risks associated with methamphetamine use disorder can escalate into life-threatening complications, including meth overdose. Why Early Recognition Matters Recognizing the signs of methamphetamine addiction early provides an opportunity to access life-saving resources such as counseling, medical detox, and behavioral therapy. Delayed action can result in worsening symptoms and more severe health risks. Physical Signs of Meth Use Meth Mouth One of the most visible signs of meth abuse is meth mouth. Severe dental problems like tooth decay, gum disease, and missing teeth are common. Methamphetamine reduces saliva production, contributing to poor oral hygiene. Untreated meth mouth can lead to long-term oral health issues. Altered Physical Appearance Prolonged meth use causes noticeable physical changes. Extreme weight loss and malnutrition occur due to reduced appetite. Skin sores from excessive scratching or picking are common among meth users. Track marks may be visible on individuals who inject meth. Behavioral Signs of Meth Use Unusual or Unhealthy Lifestyle Habits The effects of meth extend to daily routines and habits. Meth users often experience disrupted sleep patterns, staying awake for days. Personal hygiene is frequently neglected, and erratic behaviors like risky activities increase. Irrational Behaviors Using meth leads to mental health disturbances and irrational actions. Tweaking occurs during the crash phase, with heightened paranoia and anxiety. Users may engage in compulsive actions, like repetitive cleaning or disassembling objects. Poor judgment and risky decision-making are common. Cognitive and Emotional Changes Tweaking Tweaking is a critical phase in methamphetamine use disorder, marked by cognitive and emotional instability. Mood swings, paranoia, and aggressive behavior often accompany tweaking. Anxiety and agitation are heightened during this period. Recognizing Meth Addiction Symptoms and Warning Signs Understanding the signs of methamphetamine addiction is key to early intervention. Chronic meth use often results in neglect of responsibilities, relationships, and hygiene. Drug facts suggest compulsive use and withdrawal symptoms indicate addiction. Meth Addiction Treatment Treatment Options Recovery from meth addiction is possible with structured treatment. Medical detox is the first step in managing meth withdrawal safely. Behavioral therapies like cognitive-behavioral therapy (CBT) address underlying causes of addiction. Support from support groups and mental health services administration enhances long-term recovery. Supporting a Loved One with Meth Addiction Encouraging Treatment and Recovery Family members play a significant role in supporting recovery. American addiction centers emphasize the importance of emotional support and resources. Encouraging a loved one to seek help can make a difference in their recovery journey. Long-Term Effects and Risks of Meth Use Health Risks and Consequences The long-term effects of meth are life-altering and often irreversible. Prolonged use increases the risk of organ failure, chest pain, and heart attack. Meth use can lead to health risks like HIV/AIDS or hepatitis from sharing needles. Mental health conditions such as psychosis and depression frequently develop. Meth Withdrawal and Recovery Withdrawal Symptoms and Treatment Withdrawal from meth is challenging but manageable with the right support. Meth withdrawal symptoms include depression, fatigue, and intense cravings. Treatment involves medication-assisted treatment, therapy, and counseling to ease withdrawal and aid recovery. Conclusion Recognizing the signs of meth use is the first step in addressing the devastating effects of methamphetamine addiction. Physical, behavioral, and emotional symptoms often serve as warning signs, signaling the need for intervention. Ignoring these signs can lead to severe health complications, strained relationships, and irreversible damage to mental and physical well-being. Understanding the symptoms and seeking professional help can make a significant difference in an individual’s journey toward recovery. If you or someone you care about is showing signs of drug abuse, it’s essential to act swiftly. Addiction impacts not only the individual but also their family, friends, and community. Meth use can result in life-threatening consequences, including overdose, severe mental health disorders, and long-term physical deterioration. Addressing these issues early provides a better chance for recovery and minimizes further harm. Support is available, and recovery is achievable with the right combination of treatment and encouragement. Professional assistance, including meth addiction treatment, offers a structured approach to overcoming dependency. Options such as medical detox, behavioral therapies like cognitive-behavioral therapy (CBT), and participation in support groups help individuals address the root causes of addiction and build healthier coping mechanisms. These resources are vital for long-term sobriety and overall well-being. Seeking Treatment? We Can Help! At Sullivan Recovery, as an in-network provider we work with most insurance plans, such as: Tricare Blue Shield Magellan Health First Health Network The Holman Group Cigna Anthem BCBS Aetna Humana TriWest HMC Healthworks Molina UnitedHealthcare Optum UMR And More If you or a loved one are struggling with mental health challenges or substance abuse, reach out to Sullivan Recovery today. Our team of compassionate professionals is here to support your journey towards lasting well-being. Give us a call at 949-836-7180. Frequently Asked Questions 1. What are the most common signs someone is on meth? The most common signs of meth use include noticeable
