What is Ketamine Made Of? Understanding Its Chemical Makeup and Uses
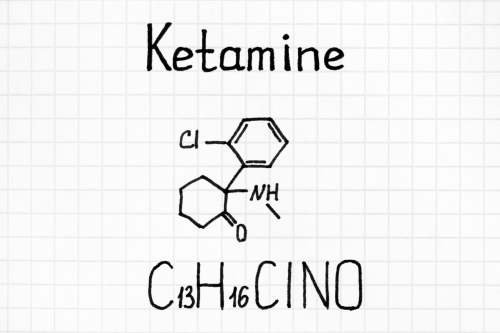
Table of Contents Seeking Drug Or Alcohol Detox? Sullivan Recovery is a leading drug and alcohol detox in Mission Viejo, California. Call Today! Clinically Reviewed By: Rachel Sweet | LMFT What is Ketamine Made Of? Understanding Its Chemical Makeup and Uses Ketamine is a synthetic compound that has gained attention for its use across various fields, from medical treatments to recreational settings. Initially developed in the 1960s as an anesthetic agent, it has evolved into a versatile substance used to treat conditions such as treatment-resistant depression, chronic pain, and post-traumatic stress disorder (PTSD). Ketamine treatment has shown efficacy for conditions like treatment-resistant depression, acting as a rapid-acting antidepressant and offering potential benefits for specific patient populations. However, it has also become a target of recreational drug abuse, raising concerns about ketamine abuse and misuse. In this article, we will explore what ketamine is made of, how it functions, and its impact on both the medical and recreational landscape. What is Ketamine? Ketamine is a medication primarily used for inducing and maintaining anesthesia during surgery. It belongs to a class of drugs known as dissociative anesthetics, which work by blocking sensory perception and inducing a state of dissociation or detachment from one’s surroundings. This unique mechanism allows ketamine to provide potent analgesic (pain-relieving) effects, making it valuable in both emergency medicine and the management of chronic pain conditions. Beyond its medical applications, ketamine is also known for its hallucinogenic and dissociative effects. These properties have contributed to its popularity as a recreational drug, where it is often sought after for the intense, out-of-body experiences it can produce. However, this recreational use comes with significant risks, including the potential for ketamine abuse and adverse health effects. What Is Ketamine Made Of? Ketamine is classified as a dissociative anesthetic, meaning it can disconnect users from their environment and bodily sensations. It is composed of the following key elements: Arylcyclohexylamine: This forms the backbone of ketamine’s chemical structure, giving it unique properties as both an anesthetic and a psychoactive substance. Chlorine and nitrogen atoms: These components play an essential role in making ketamine effective for both therapeutic and dissociative uses. Through laboratory ketamine production processes, this compound is synthesized into several forms, including a liquid, powder, and nasal spray. Each form serves different purposes in medical or recreational settings. For example, liquid ketamine is used in ketamine infusion therapy, while powder ketamine may be abused recreationally. Ketamine as a Medical Tool Initially, ketamine was widely used in veterinary medicine and for surgical procedures because of its powerful anesthetic properties. Its effectiveness as an anesthetic agent lies in its ability to provide pain relief without significantly suppressing breathing—one of the risks associated with other anesthetics like opioids. In modern psychiatry, ketamine has gained prominence for treating treatment-resistant depression, particularly because of its rapid onset of antidepressant effects. While most traditional antidepressant medications take weeks to show improvements, ketamine can relieve depressive symptoms within hours. This makes it an invaluable tool for treating individuals experiencing acute suicidal ideation. Ketamine treatment is especially noted for its efficacy in specific patient populations and its potential as a rapid-acting antidepressant. Ketamine infusion therapy: Administered intravenously under medical supervision, this therapy has shown great promise in alleviating symptoms of chronic pain and various mental health disorders, including post-traumatic stress disorder (PTSD) and certain mental health conditions that don’t respond well to other treatments. Recreational Use of Ketamine as a Recreational Drug and Ketamine Abuse While ketamine offers significant therapeutic benefits, its hallucinogenic effects have also made it a popular recreational drug. In these settings, ketamine is often used for the dissociative “high” it produces, but repeated or excessive use can lead to ketamine abuse. Recreational users risk experiencing adverse effects such as: Elevated blood pressure Bladder damage (also known as ketamine-induced cystitis) Disorientation and hallucinogenic effects Dependence and ketamine overdose Given these risks, ketamine is classified under the Controlled Substances Act as a Schedule III controlled substance. This designation reflects its potential for abuse and dependence, while still recognizing its medical value when used properly. How Ketamine Works in the Brain Ketamine works by blocking NMDA (N-methyl-D-aspartate) receptors in the brain. These receptors are involved in pain transmission and mood regulation. By inhibiting their activity, ketamine produces both analgesic effects and mood-elevating properties, making it particularly useful for people with treatment-resistant depression and chronic pain. Ketamine treatment leverages this mechanism of action to provide rapid-acting antidepressant effects, making it a valuable option for specific patient populations. Interestingly, ketamine also interacts with opioid receptors, adding another layer to its effectiveness as a pain relief medication. This combination of effects allows it to treat conditions that may not respond to traditional painkillers or antidepressants. Administration of Ketamine Ketamine treatment can be administered in various ways, depending on the medical need: Ketamine infusion therapy: Delivered intravenously, this is the most common method for treating mental health conditions like depression and PTSD. Nasal spray: This form of ketamine treatment, often used in outpatient settings, offers an alternative for individuals with depressive symptoms. Oral ketamine: Less common but sometimes prescribed for chronic conditions. The dosage is typically calculated using metrics like mg/kg to ensure patients receive an appropriate amount. Sub-anesthetic doses are often used to minimize the risk of side effects while still achieving the desired therapeutic effects. Ketamine Infusion Therapy Ketamine infusion therapy is an innovative treatment approach that involves the administration of ketamine in a controlled medical setting to manage various medical and psychiatric conditions. This therapy has shown remarkable efficacy in addressing treatment-resistant depression, post-traumatic stress disorder (PTSD), and chronic pain. Typically, ketamine infusion therapy involves the intravenous administration of ketamine in a series of sessions. The goal is to achieve rapid relief from symptoms, often within hours, which is particularly beneficial for individuals who have not responded to traditional antidepressant medications. The therapy is usually performed under the guidance of a trained healthcare professional, ensuring safety and effectiveness. In many cases, ketamine infusion therapy is used in conjunction with other
Step 1 in NA: Embracing Powerlessness for Recovery
Table of Contents Seeking Drug Or Alcohol Detox? Sullivan Recovery is a leading drug and alcohol detox in Mission Viejo, California. Call Today! Clinically Reviewed By: Rachel Sweet | LMFT Step 1 in NA: Embracing Powerlessness for Recovery When embarking on the journey of Narcotics Anonymous (NA), participants are introduced to the 12-step program—a structured path toward recovery from substance use disorders. The first step serves as the foundation for the entire program, where individuals recognize the need for help and acknowledge their lack of control over addiction. Step 1 in NA reads: “We admitted we were powerless over our addiction—that our lives had become unmanageable.” This is a profound moment of surrender, signaling a shift from denial to acceptance. It helps people struggling with substance abuse recognize that change begins only after they acknowledge the limitations of their own willpower and their most sincere desire to stop using drugs. What Is the First Step in Narcotics Anonymous? At its core, Step 1 in NA requires an honest admission that addiction has taken control, leaving life in chaos. This step emphasizes personal responsibility while also teaching that reliance on sheer willpower alone is not enough. Members come to realize that they must admit complete defeat, acknowledging that they can no longer handle drugs or other mood-altering chemicals without falling deeper into destructive behaviors. The admission, though difficult, is a necessary foundation. From here, participants can begin the healing process—learning to live without drugs and reconnecting with others in mutual support groups. For many, acknowledging that they are powerless over addiction is both daunting and liberating, marking the beginning of recovery from an otherwise overwhelming struggle. Understanding the Meaning Behind Step 1 Step 1 serves as a moment of truth. Admitting powerlessness over addiction is only half the truth; many people struggling with addiction spend years trying to control their behavior, only to find that the harder they fight, the more unmanageable their lives become. This pattern can leave them emotionally drained, leading to feelings of spiritual pain and complete defeat. However, accepting this defeat is not about failure—it’s about laying down the burden of constant struggle. It represents a starting point for change. Admitting powerlessness opens the door to asking for help and acknowledging the need for a power greater than oneself. Whether that higher power is spiritual, community-based, or simply the NA fellowship, this realization plays a key role in rebuilding lives. The Origins of the 12-Step Model The 12-Step model has its roots in the early 20th century, when Bill Wilson and Dr. Bob Smith founded Alcoholics Anonymous (AA) in 1935. Both men, recovering alcoholics themselves, sought to create a structured program that could help others achieve sobriety and maintain long-term recovery. Their approach was grounded in their own experiences and emphasized spiritual growth, self-reflection, and mutual support. Narcotics Anonymous (NA) adopted the 12-Step model in 1953, tailoring it to meet the specific needs of individuals struggling with narcotics addiction. This adaptation allowed NA to address the unique challenges faced by those addicted to drugs other than alcohol. Today, the 12-Step model is a cornerstone of numerous recovery organizations and mutual support groups worldwide, including both NA and AA. Its principles continue to guide countless individuals on their journey to recovery, offering a path to healing and a supportive community. How Addiction Leads to Lives Had Become Unmanageable The phrase “our lives had become unmanageable” is central to Step 1. Addiction doesn’t just impact the physical body; it also wreaks havoc on relationships, finances, mental health, and emotional well-being. People caught in the grip of addiction may lose their jobs, alienate family members, or find themselves isolated from recovery houses or recovery communities that could offer support. Those who try to stop using substances often experience withdrawal and cravings—an overpowering desire to use again despite their best intentions. The mental obsession with substance use leads to repeated relapse, reinforcing the feeling that recovery is impossible through personal effort alone. This cycle highlights the need to embrace powerlessness and the inability to manage one’s own lives to begin moving forward. The Dangers of Dishonesty in Recovery Dishonesty can be a significant barrier to recovery. When individuals struggling with addiction are not truthful with themselves or others, they create a sense of separation and isolation that can impede their progress. This dishonesty often leads to feelings of guilt, shame, and anxiety, which can trigger cravings and increase the risk of relapse. In the context of the 12-Step program, dishonesty can prevent individuals from fully acknowledging their powerlessness over addiction and the unmanageability of their lives. This lack of honesty makes it difficult to surrender to the disease of addiction and seek the necessary help. Moreover, dishonesty can damage relationships with sponsors, therapists, and support group members, undermining the sense of community and mutual support that is crucial for recovery. Embracing honesty is essential for building trust, fostering connections, and creating a solid foundation for long-term recovery. The Mental and Spiritual Awakening Aspects of Recovery Step 1 also addresses both the mental aspect and spiritual part of addiction. The physical aspect refers specifically to the compulsive use of drugs and the inability to stop using once initiated, emphasizing that this aspect is a significant part of the overall struggle with addiction. Many participants describe feeling lost, as though life lacks meaning or direction. This emotional emptiness often drives substance abuse in the first place, as drugs become a temporary solution to deeper issues. Through NA, participants learn that the spiritual awakening achieved in recovery brings freedom from this emptiness. Surrendering to powerlessness allows them to confront their exact nature and begin rebuilding their sense of self. This step also invites them to explore what spiritual disease means—understanding that addiction is more than a physical problem. Healing requires addressing the emotional and spiritual dimensions of recovery as well. Surrender as a Path to Freedom In Narcotics Anonymous, surrender is not about giving up but about realizing they have absolutely no choice
